Want to be more informed about your insurance and healthcare? Use the Tristar Member app to look up the status of a claim, review your current coverage, and research personal health and wellness topics. Because this app requires a username and password, your personal health info will be kept secure when you’re not using the app.
Features:
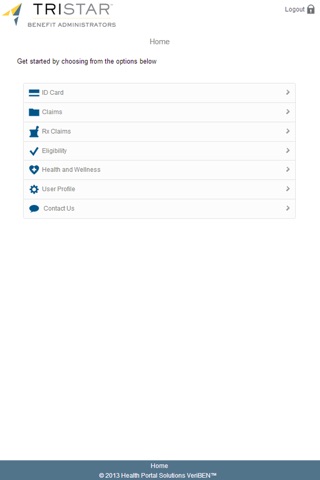
ID Card – View your virtual member ID card and show it to your doctor.
Claims – Review your recent doctor visits and check the status of your claims.
RX Claims – Look up your recent prescription claim details.
Eligibility – See your coverage info and your In-Network and Out-of-Network expenses.
Health and Wellness – Get up-to-date health news, tips, and videos that can help you live a healthier lifestyle.
User Profile – Make changes to your contact info and account.
Requirements (Apple): The Tristar Member App is compatible with the iPhone, iPad, and iPod Touch. Requires iOS 6.1+.
About Tristar Benefit Administrators
Tristar delivers outstanding administrative services for employer benefit plans. We provide personalized customer service, efficient processing of claims, and sophisticated and secure online tools 24/7 to plan members. For more info, check out our website at www.tbahealth.com.